Why is asthma prevention and treatment difficult? Small airway inflammation is a major challenge!
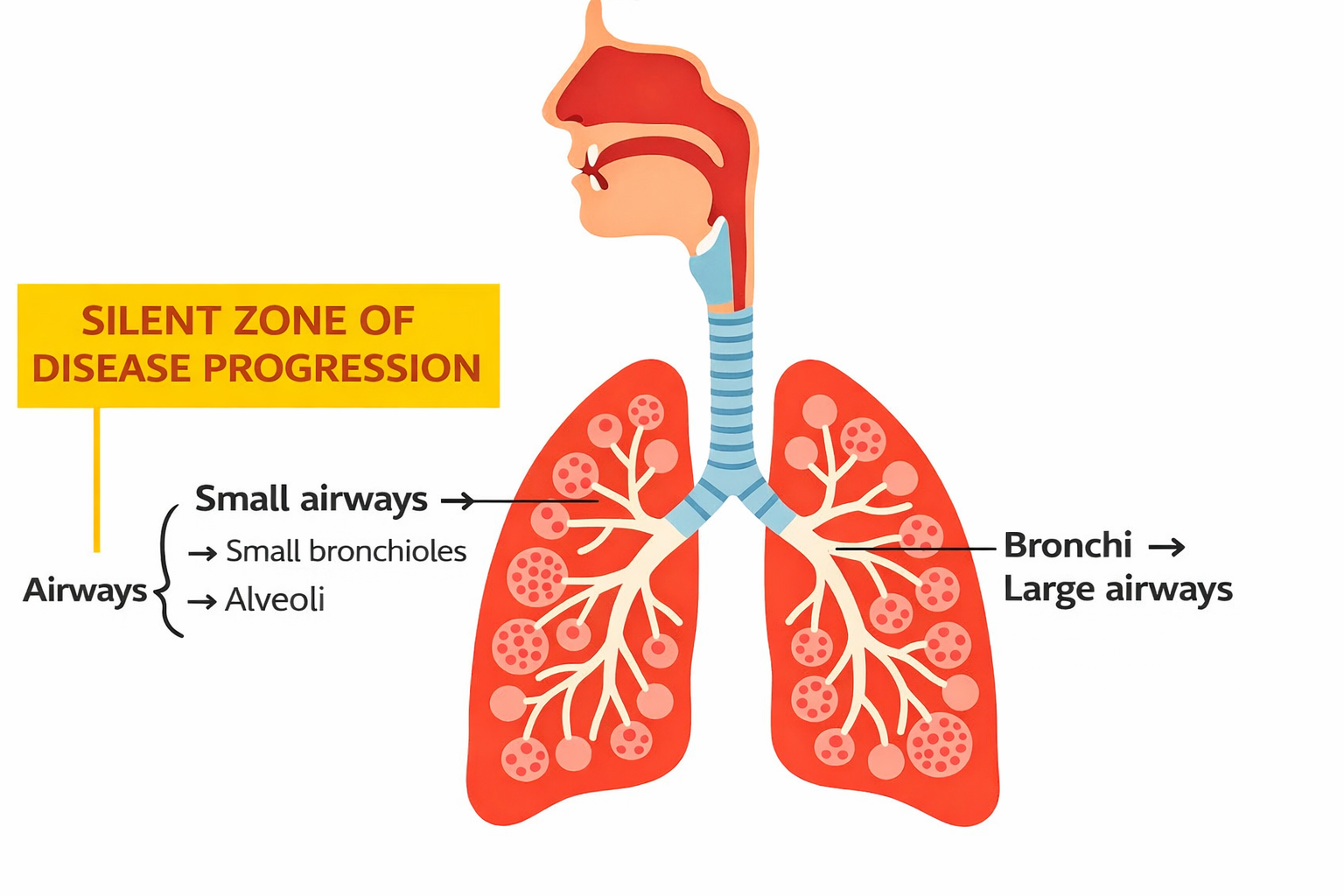
Asthma is a recurring and difficult-to-cure disease, a dilemma faced by many patients and doctors alike. Traditional treatments often focus on controlling inflammation and symptoms in the large airways, but tend to overlook a hidden yet crucial "battlefield"—the small airways.
Inflammation within the small airways is a significant factor contributing to poor asthma control, frequent acute exacerbations , and the potential progression to severe asthma.
Why is small airway inflammation so insidious and difficult to prevent and treat?
➡ 1. The essence of refractory and severe asthma is mainly small airway inflammation.
First, small airway inflammation is difficult to detect and often occurs late , while routine lung function and FeNO tests mainly detect large airway lesions.
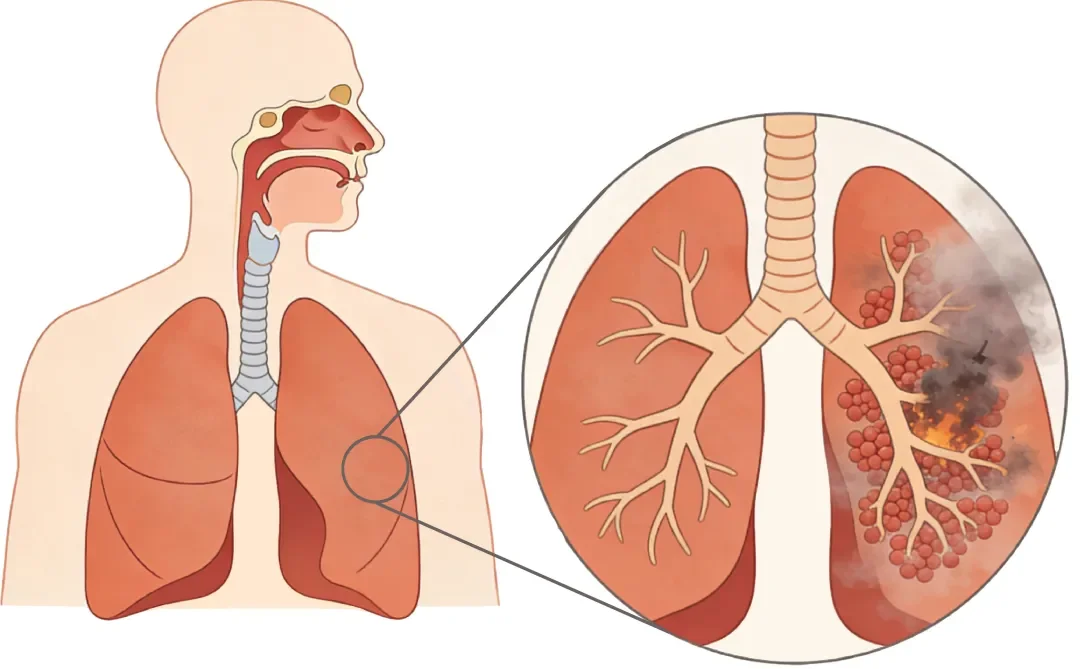
Secondly, administering medication through small airways is particularly difficult , as oral inhalation or systemic hormone delivery is challenging, and most of the hormones are consumed en route to the alveoli in the small airways.
➡ 2. The multifocal nature of small airway inflammation is also one of the reasons why asthma is difficult to prevent and treat .
It can spread downwards from the upper airway , or it may originate from the extension of chronic inflammation in the large airways, and it is even closely related to systemic immune disorders . However, because of its deep location and difficulty in being detected by routine examinations, it is often overlooked. (See this issue's Clinical Progress section for details)
Identification Tools: Inflammation Manager® Breath Analyzer and Monoclonal Antibodies
How to overcome the diagnostic blind spot of small airway inflammation? Precision medicine technology has solved this problem.
I. The new variable flow breath test technology developed by Shangwo Medical can detect small airway inflammation early and conveniently.
This technology can non-invasively identify type 2 small airway inflammation by measuring the exhaled nitric oxide concentration (FeNO200/CaNO).
At the same time, it can be used for daily monitoring of inflammation in the upper and lower airways, as well as the large and small airways, in the home environment, thereby building an online and offline, in-hospital and out-of-hospital management system.
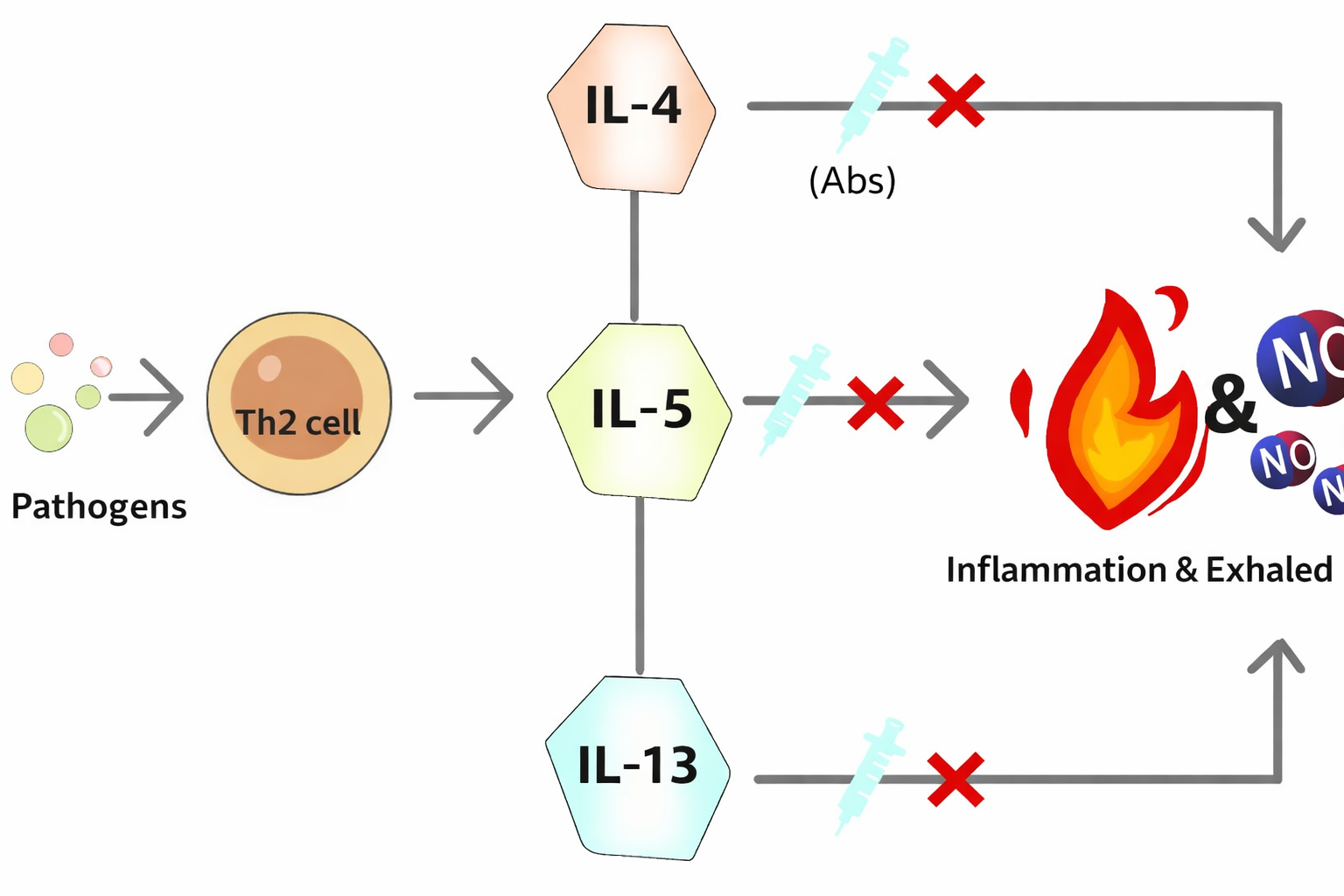
Second, monoclonal antibody drugs developed by international pharmaceutical giants can enter the small airways and other sites of inflammation.
Both of these technologies have been widely and successfully applied in hospitals.
More notably, CaNO testing is of great value in assessing the use and efficacy of biologics (such as anti-IL-4, IL-5, and IL-13 monoclonal antibodies) in these patients . It can provide doctors with dynamic inflammatory data, helping to achieve personalized and precise treatment and avoid undertreatment or overtreatment.
Case sharing - No. 3
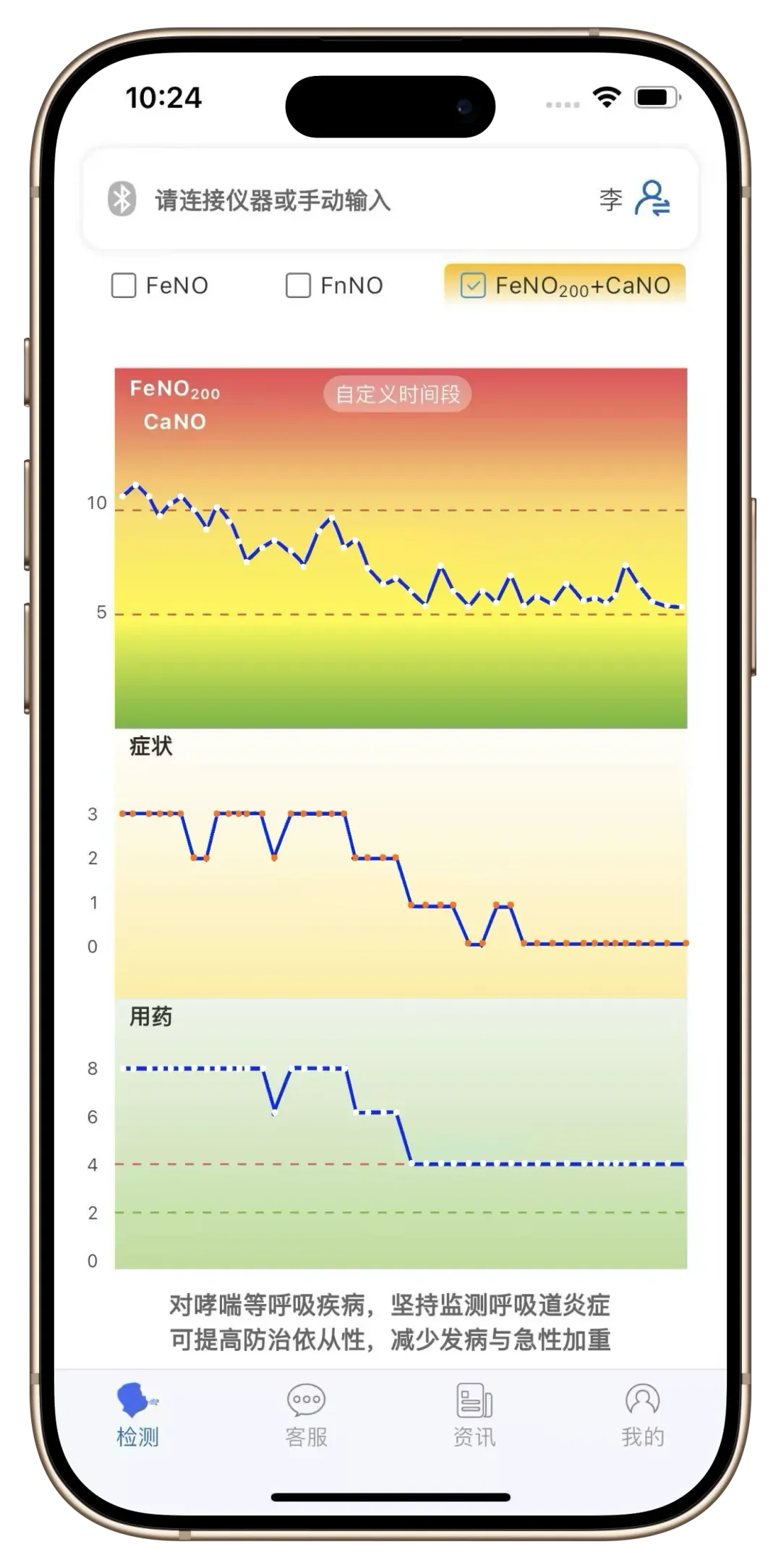
Xiao Li is a ten-year asthma patient who has been monitoring FeNO and using inhaled corticosteroids (ICS) to control his asthma.
Recently, Xiao Li noticed that although her FeNO level remained stable at around 25 ppb , her symptoms did not improve (after the second dotted line in Figure 1 report) , and she frequently experienced coughing, wheezing, and difficulty breathing . Looking back on her daily life, she had effectively avoided allergens and taken medication regularly and correctly . To avoid delaying her treatment, she immediately consulted a doctor through the Yan Guan Jia® App. After understanding her situation, the doctor recommended that she use the Yan Guan Jia® Breathalyzer (TM) for a combined large and small airway examination to observe whether there was inflammation in the small airways.
As shown in Figure, Xiao Li's CaNO value was 10.7 ppb , which is more than half higher than the normal value (cutoff point 5 ppb). This indicates that she has small airway inflammation, and it is recommended to increase her daily monoclonal antibody therapy.Daily combined examination of both large and small airways is conducted to monitor the efficacy of ICS and monoclonal antibodies .
After a period of treatment, Xiao Li's CaNO value decreased significantly (5.6 ppb) (see Figure 2) , while FeNO remained at around 25 ppb (after the second dotted line in Figure 1) , and his symptoms were also relieved, indicating that the inflammation in both the large and small airways was effectively controlled.
In summary, long-term control of asthma requires establishing a "global airway" concept, especially incorporating the small airways—a hidden battleground—into the core of monitoring and treatment , and implementing a combined intervention strategy for both large and small airways. Only in this way can we break free from the predicament of recurrent attacks and move towards a truly stable and free breathing life.
References:
【1】Toumpanakis D, Usmani OS. Small airways in asthma: Pathophysiology, identification and management. Chin Med J Pulm Crit Care Med. 2023.
【2】Overview of the Respiratory System: Function and Structure.
[3] Wang Xuechen, Jin Jianmin. Chinese Journal of Tuberculosis and Respiratory Diseases, 2023, 46(8): 824-828.
【4】Mustafa Abdo, et al. J Asthma Allergy. 2021 Jul 13.
【5】Marcello Cottini, et al. J Allergy Clin Immunol Pract. 2020 Mar.
【6】Toumpanakis D, Usmani OS. Small airways in asthma: Pathophysiology, identification and management. Chin Med J Pulm Crit Care Med.
【7】Wang, Jing et al. “The value of concentration of alveolar nitric oxide in diagnosing small airway dysfunction in patients with stable asthma.” The clinical respiratory journal, 10.1111/crj.13565. 12 Dec.