Why are small airways a challenge in the prevention and treatment of asthma?
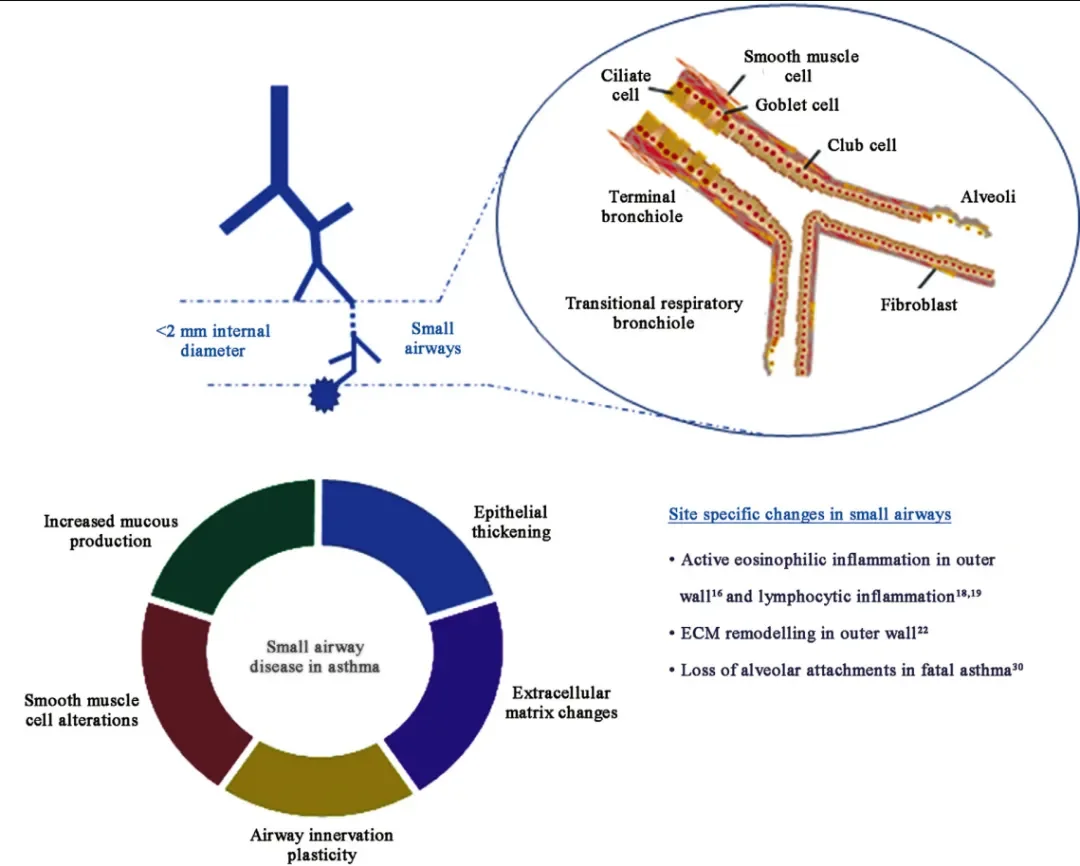
In recent years, the role of small airways (airways with an internal diameter of less than 2 mm) in the pathogenesis of asthma has gradually gained attention. However, due to their insidious nature and difficulty in detection, small airway inflammation has become a key challenge in the prevention and treatment of asthma.
1- Small airway inflammation is multifocal.
The core pathology of small airway inflammation is inflammatory infiltration and airway remodeling. Its pathogenesis involves a series of structural remodeling processes, including increased mucus secretion, goblet cell metaplasia, epithelial shedding and basement membrane thickening, smooth muscle hyperplasia and hypertrophy, and changes in the extracellular matrix. This process is characterized by the coexistence of type 2 and non-type 2 inflammation: type 2 inflammation, driven by cytokines such as IL-4, IL-5, and IL-13, is eosinophil infiltration and is significantly associated with severe small airway dysfunction (SAD); non-type 2 inflammation is predominantly neutrophilic and may be associated with elevated interferon-γ levels. Due to their narrow lumen, thin walls, and abundant smooth muscle, small airways are highly susceptible to damage under sustained inflammation, leading to epithelial injury, abnormal smooth muscle proliferation, and collagen deposition, thereby causing airway narrowing and wall thickening.
Small airway inflammation is multifocal, originating from the upper airway, large airway, and even the whole body. Allergic rhinitis can trigger systemic airway inflammation by upregulating adhesion molecules, and is an independent risk factor for small airway dysfunction in asthma patients. Inflammation in the proximal large airways can also spread to the peripheral small airways via cytokines. In addition, systemic pro-inflammatory states such as obesity and smoking, as well as systemic activation of Th2 cells (such as increased circulating IgE and memory B cells), can exacerbate local lesions in the small airways through inflammatory factors, forming a vicious cycle of inflammation and remodeling.
More importantly, the small airways are remarkably insidious. Although they comprise 98.8% of the total lung volume, their "silent zone" nature means that early lesions often present without typical symptoms, leading to a high rate of missed diagnoses. The latest ATLANT IS study published in *The Lancet Respiratory Medicine* found that even in patients with well-controlled asthma symptoms, approximately one-third still exhibit small airway dysfunction, and their risk of acute exacerbations increases independently by more than two times in the following year. This profoundly reveals the "difficult to detect" nature of the small airways, posing a significant challenge to the clinical assessment and prevention of asthma.
2- Clinical challenges in small airway detection
Previously, due to technological limitations, asthma research focused primarily on the large airways, leading to the long-term neglect of the crucial small airways. With technological advancements, research has revealed that asthma patients with concurrent small airway dysfunction exhibit unique clinical phenotypes: prominent nocturnal and exercise-induced asthma symptoms, significantly increased risk of emergency room visits and hospitalizations, poorer treatment response, and the need for higher doses of glucocorticoids. Studies by Cottini et al. have clearly demonstrated that high FeNO levels, female sex, smoking, old age, overweight, and exercise-induced asthma symptoms are independent predictors of severe acute exacerbation (SAD).
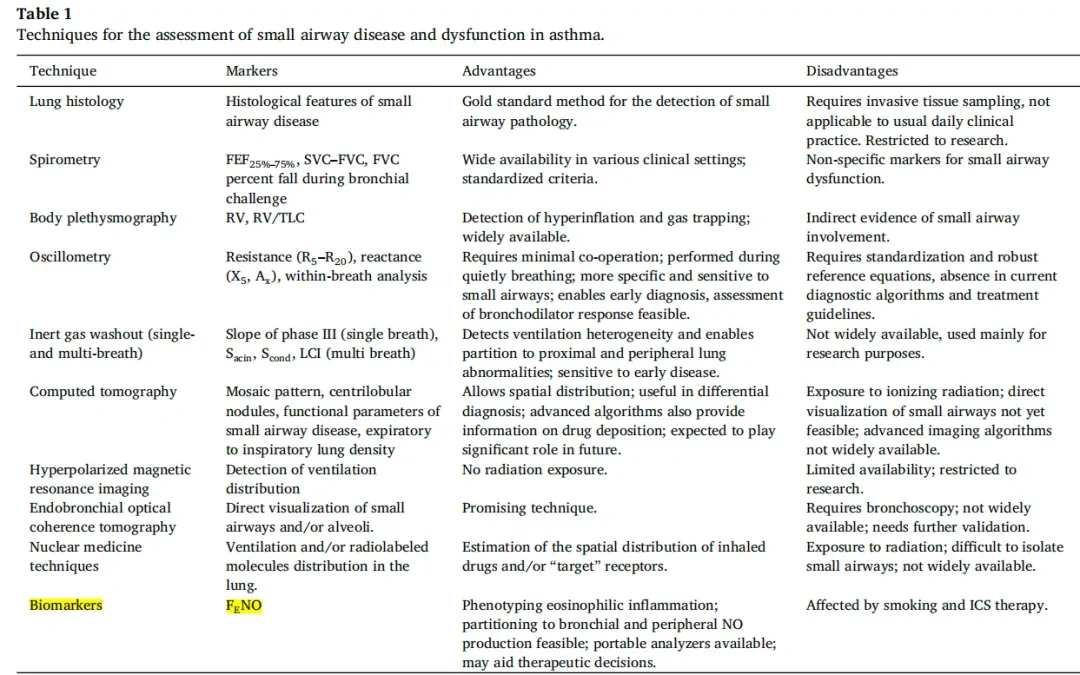
However, small airway function testing still faces challenges: routine pulmonary function tests are not sensitive enough for early lesions; pulse oscillation method is more sensitive to small airways but lacks standardized guidelines; CT can show airway remodeling but cannot dynamically assess function; inert gas elution (such as LCI) and induced sputum analysis are mostly limited to research applications.
In recent years, the development of non-invasive airway inflammation detection technology has brought new breakthroughs to small airway assessment, with FeNO testing becoming a routine clinical procedure for asthma. FeNO50 primarily reflects type 2 inflammation in the large airways, but a low value cannot rule out small airway inflammation. In contrast, alveolar NO concentration (CaNO) more accurately reflects the level of small airway inflammation. Studies have shown that elevated CaNO is significantly associated with refractory asthma, nocturnal symptoms, and frequent acute exacerbations related to small airway dysfunction. To achieve accurate assessment of the small airways, it is necessary to combine multiple detection methods and jointly analyze the inflammatory characteristics of both large and small airways, thereby providing a basis for the development of individualized treatment plans.
3- Challenges in the prevention and treatment of small airways
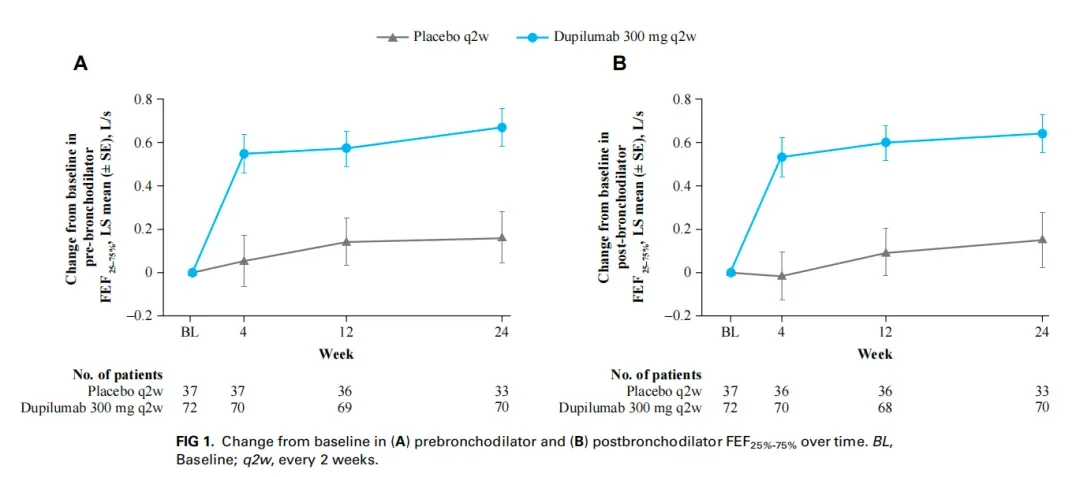
Patients with asthma and small airway dysfunction face significant treatment challenges, with conventional ICS or ICS-LABA therapy limited in efficacy due to the difficulty in effectively depositing drug particles into the peripheral small airways. Studies have shown that these patients have unique benefits from biologic therapy, particularly those with severe SAD, which may indicate a specific eosinophilic asthma phenotype. Recent clinical evidence shows that dupilumab, targeting the IL-4/IL-13 pathway, can significantly improve small airway function and structure: in 109 patients with moderate to severe asthma (baseline FeNO ≥ 25 ppb), treatment not only improved small airway function indicators such as FEF 25%-75% and FEV1/FVC, and reduced airway resistance parameters such as R5-R20, but also reduced airway wall thickness and gas retention, as confirmed by high-resolution CT. Notably, changes in FeNO were significantly correlated with improvements in airway function/structure, confirming that inhibiting type 2 inflammation is a key mechanism for improving small airway lesions.
Summary
In summary, the core essence of refractory and severe asthma lies in small airway inflammation. Firstly, small airway inflammation itself is difficult to detect early, as routine pulmonary function tests and FeNO tests primarily reflect large airway lesions. Secondly, drug delivery to the small airways is particularly challenging; after oral inhalation and systemic corticosteroid administration, the drugs are consumed along their path to the small airways and alveoli. Current precision medicine technologies have successfully addressed these challenges: on the one hand, Shangwo Medical's variable flow breath test technology can conveniently and early detect small airway inflammation; on the other hand, biologics developed by international pharmaceutical giants can precisely target the small airways and other sites. These technologies are currently widely used clinically with significant results.
References:
1. Galant SP, Kuks PJM. Assessment of the role of small airway dysfunction in relation to exacerbation risk in patients with well controlled asthma (ATLANTIS): an observational study. Lancet Respir Med. 2025 Nov;13(11):990-1000.
2. Jayasooriya SM, Devereux G, Soriano JB, Singh N, Masekela R, Mortimer K, Burney P. Asthma: epidemiology, risk factors, and opportunities for prevention and treatment. Lancet Respir Med. 2025 Aug;13(8):725-738.
3. Toumpanakis D, Usmani OS. Small airways in asthma: Pathophysiology, identification and management. Chin Med J Pulm Crit Care Med. 2023 Sep 13;1(3):171-180.
4. Siora A, Vontetsianos A. Small airways in asthma: From inflammation and pathophysiology to treatment response. Respir Med. 2024 Feb;222:107532.
5. Liang Guiju, Chen Bi, Zhu Jiechen, Meng Ziqi, Zhu Shuyang . Correlation between alveolar nitric oxide and small airway function in asthmatic patients [J]. Practical Medicine Journal , 2022, 38(6): 767-772.
6. Washko GR, Lipworth BJ. Effect of dupilumab on small airways measured by airway oscillometry in VESTIGE. J Allergy Clin Immunol. 2025 Nov;156(5):1209-1218.