Patient-Hospital Community | Why is Asthma Prevention and Treatment Difficult? The Biggest Culprit is Sinusitis!
Many asthma patients face this problem: despite diligently taking medication and avoiding allergens, symptoms such as coughing, chest tightness, and wheezing still recur, significantly reducing their quality of life .
Why is asthma so difficult to "control"? In addition to the poor adherence to treatment mentioned earlier ( Medical and Patient Home | How to use the Inflammation Manager® Breathing Device and App to check treatment adherence? ) , a often overlooked "culprit" is quietly at work - sinusitis (mainly eosinophilic chronic sinusitis) .
Sinusitis and asthma are co-occurring diseases . Epidemiological studies show that approximately 50% of asthma patients also have sinusitis. 90% of severe asthma patients have thickened sinus mucosa. The prevalence of asthma in the general population is 5%-8%, while it is 10%-30% in sinusitis (see this issue's Clinical Advances for details).
It can be said that without a healthy nose, it is difficult to manage the lungs .
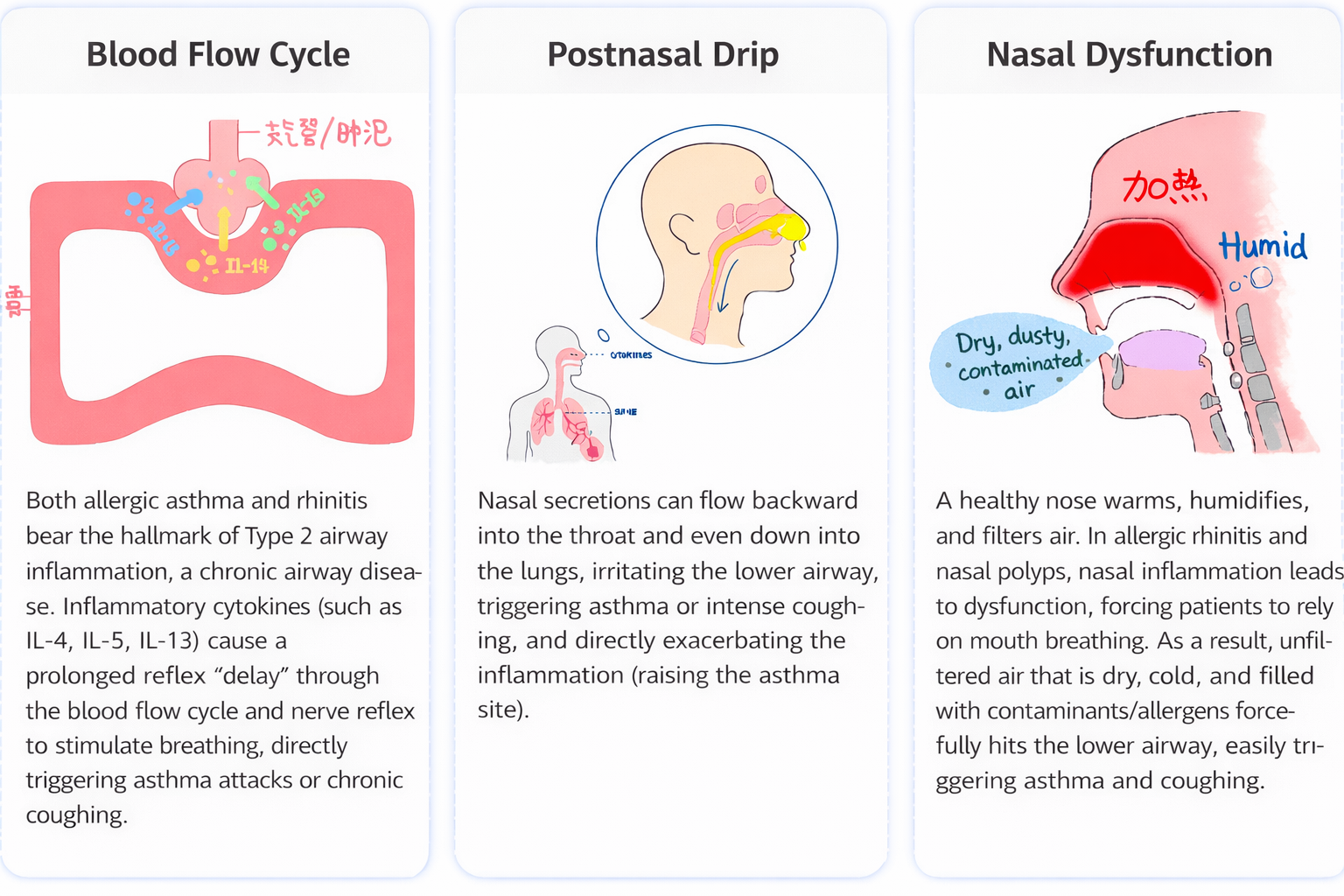
Why is sinusitis a "difficult-to-treat culprit" for asthma?
I. The core concept is "one airway, one disease ".
This concept holds that the human respiratory tract begins in the nasal cavity, passes through the sinuses, pharynx, trachea, and continues to the bronchi and alveoli . Although it is anatomically divided into upper and lower parts, it is a continuous and unified whole in terms of embryonic origin, tissue structure, physiological function, and pathological response .
Therefore, when a disease (especially allergic or eosinophil-associated type 2 inflammation) attacks one part, the other part will inevitably be affected as well.
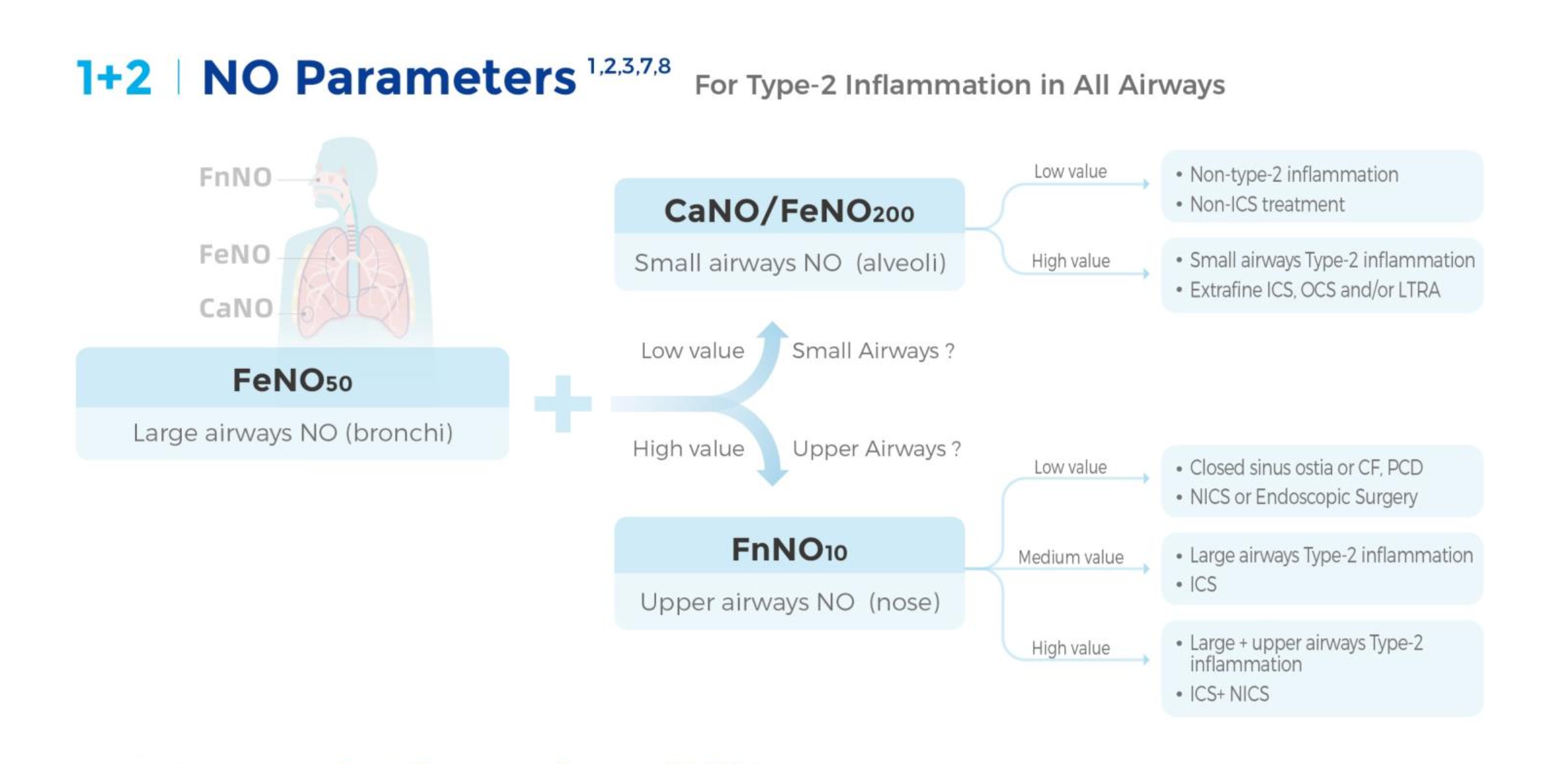
II. Key to Precise Prevention and Treatment: Identifying Inflammation in the Upper and Lower Airways
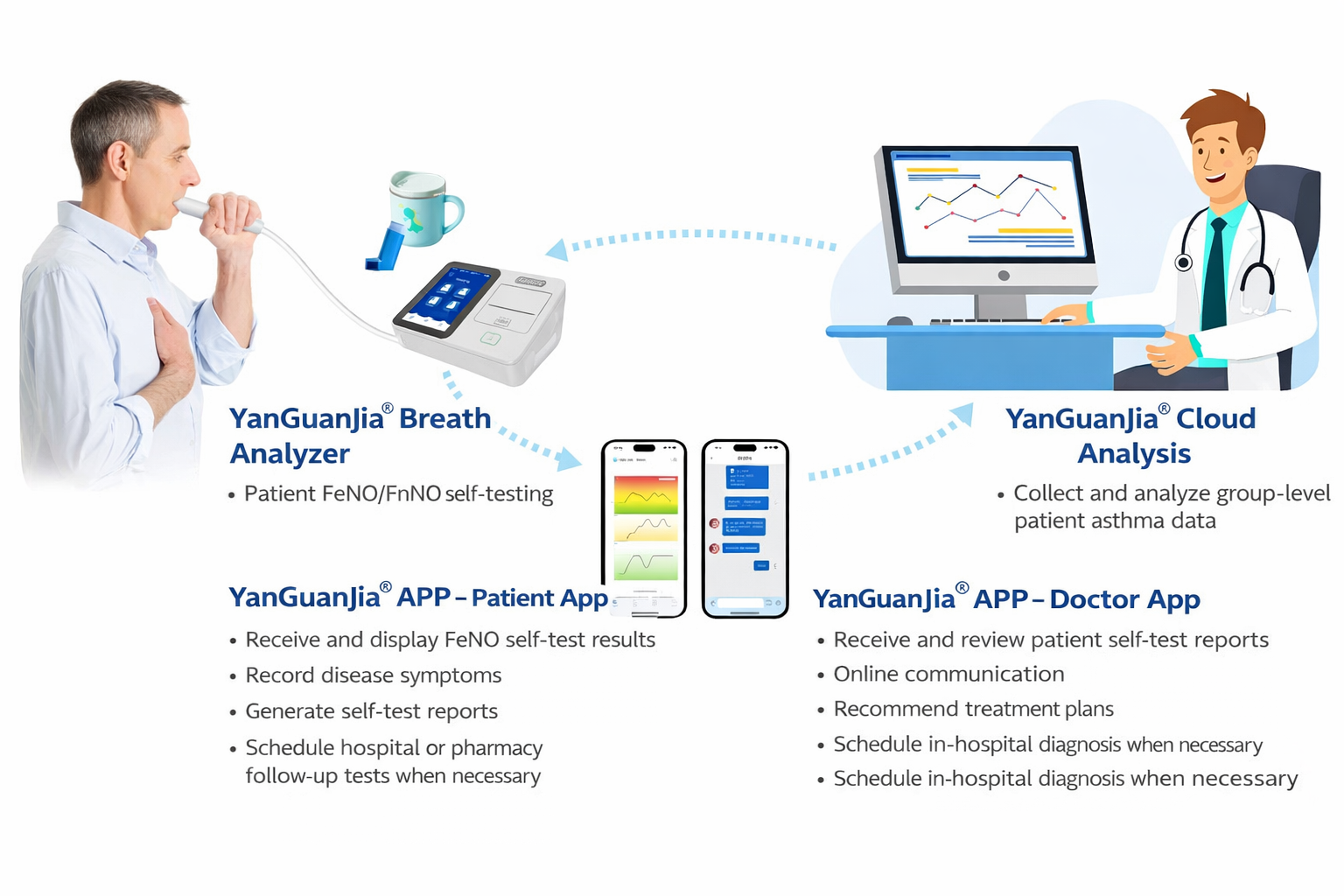
Given the close link between asthma and sinusitis, treating asthma alone while neglecting the assessment and management of the sinuses is tantamount to "treating the symptoms but not the root cause ." Modern medicine emphasizes integrated assessment, treatment, and management of the upper and lower airways , with the core tool being the combined detection of exhaled nitric oxide (FeNO + FnNO) in the upper and lower airways.
The Inflammation Manager® Breath Aspirator (TM series) developed by Sunvou Medical fully meets clinical and home management needs.
Case sharing
Mr. Zhang, 35 years old, was diagnosed with asthma two months ago. His main symptoms are wheezing after daytime activities and coughing at night, which affects his sleep.
Initial consultation (week 0):
The patient presented with cough and wheezing. The doctor performed an exhaled nitric oxide (FeNO) test, which showed a result of 89 ppb , clearly indicating significant type 2 inflammation in the lower airways . Based on the typical symptoms, a diagnosis of asthma was made. Treatment with inhaled corticosteroids/long-acting β2-agonists (ICS/LABA, such as Symbicort) was recommended, along with strict avoidance of allergens.
Treatment follow-up (weeks 1-4):
Although he strictly followed the doctor's instructions for medication, Mr. Zhang's airway inflammation and symptoms were not well controlled after 4 weeks of treatment.
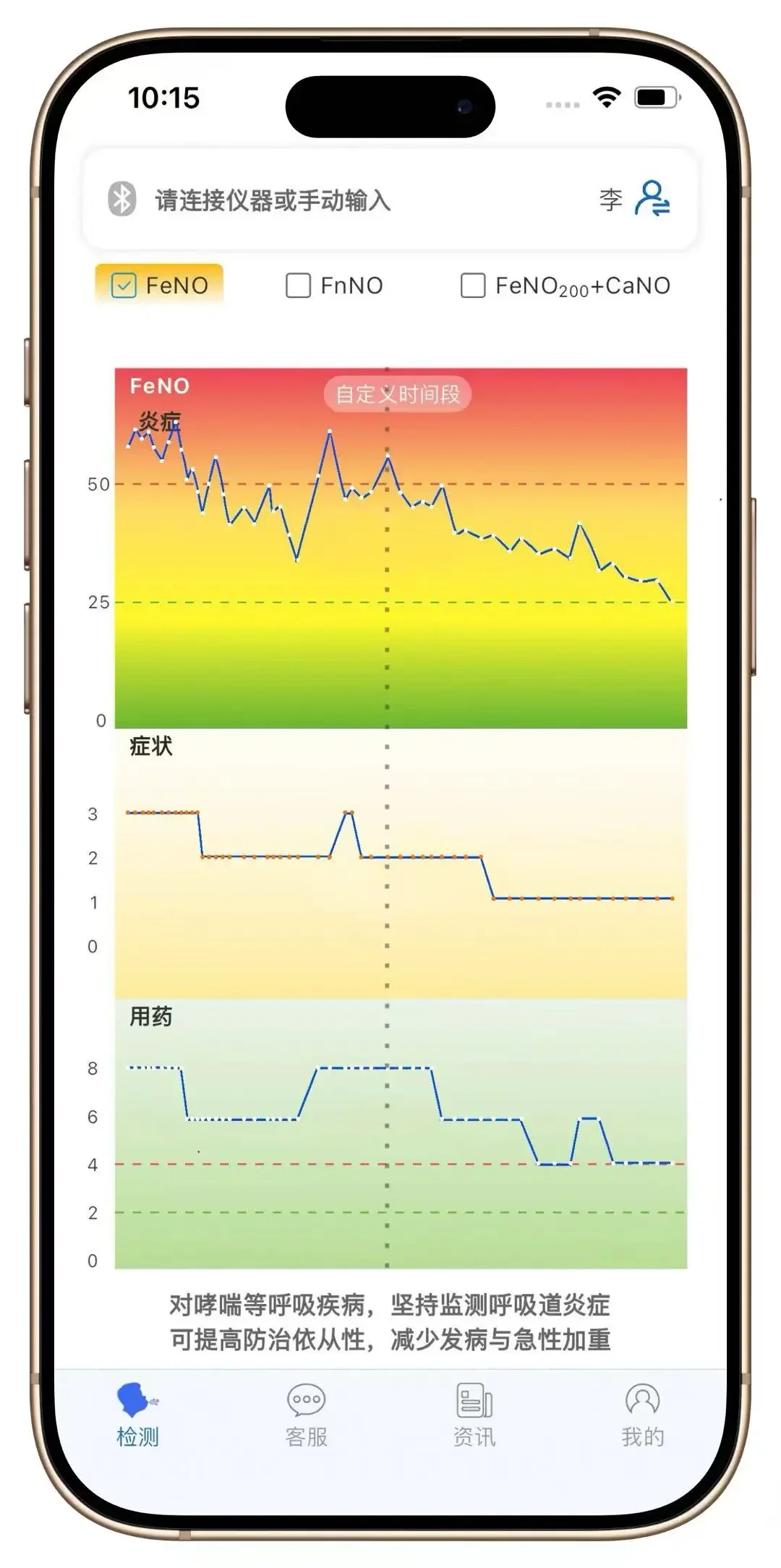
Figure 1 shows the daily FeNO monitoring curve (before the first dashed line), which indicates that the FeNO value fluctuates drastically (30-80 ppb) and is accompanied by symptoms that come and go .
During the follow-up examination, the patient added descriptions of symptoms such as nasal congestion and runny nose. The doctor then performed a combined expiratory breath test of the upper and lower airways and a sinus CT scan . The results showed that FeNO was 78 ppb, still high; while FnNO was as high as 900 ppb, indicating severe type 2 inflammation in the upper airway . Furthermore, the sinus CT scan confirmed thickening of the bilateral ethmoid and maxillary sinus mucosa, characteristic of type 2 chronic sinusitis. Based on this, nasal corticosteroids (fluticasone propionate) were added to the original treatment plan.
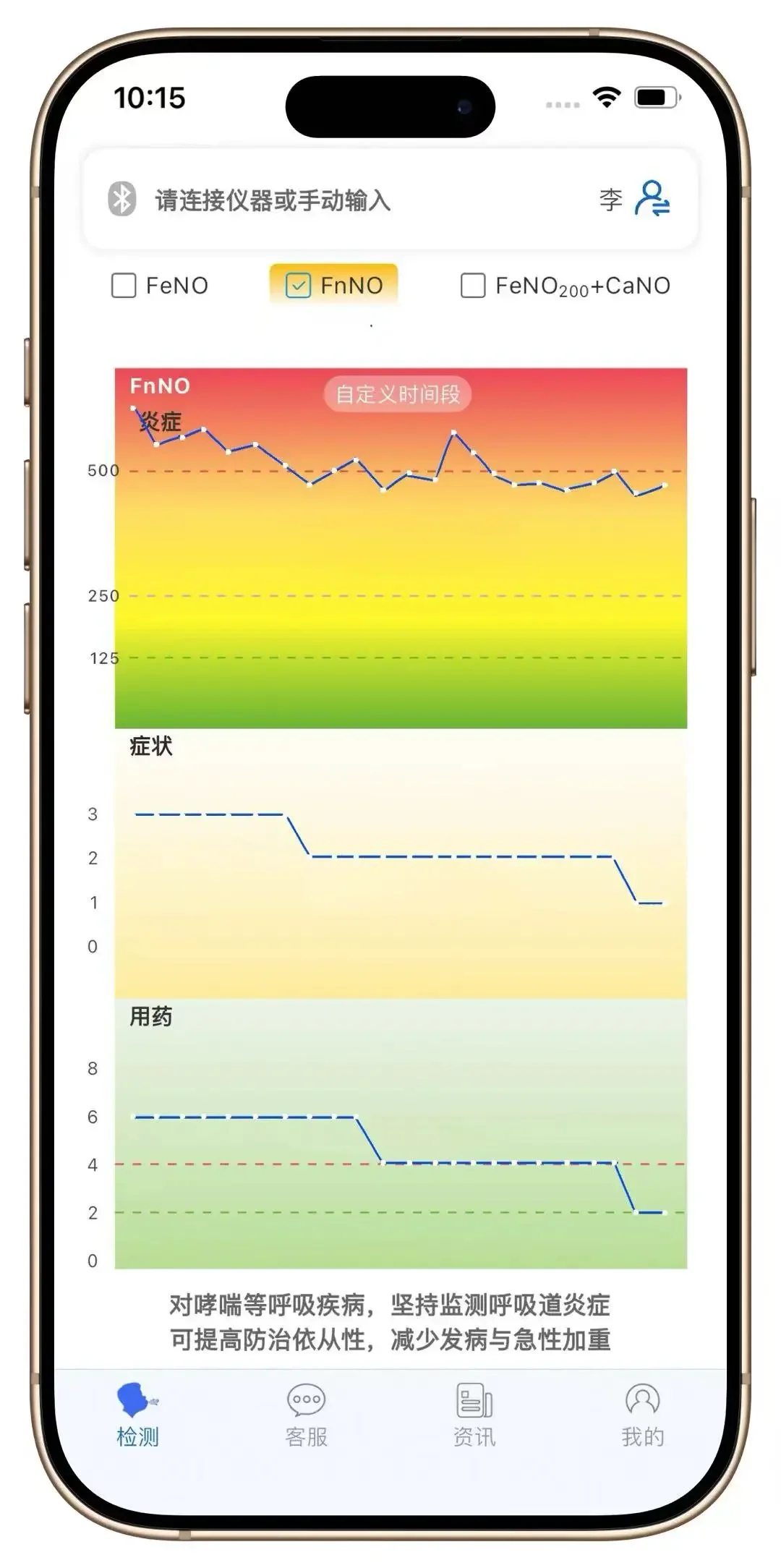
After adjusting the treatment plan, the patient's FeNO value gradually stabilized (after the first dotted line in Figure 1), and the symptoms were relieved, with bronchitis effectively controlled. Simultaneously, the FnNO value slowly decreased to a reasonable range, and nasal discomfort significantly improved (Figure 2).
Therefore, by using the key of combined upper and lower airway expiratory testing (FeNO+FnNO) , we can accurately detect airway inflammation and implement a combined strategy of "treating both upper and lower airways" to truly achieve long-term, stable control of asthma and restore freedom and smoothness to breathing.
References:
[1] Peng Min, Zhang Danmei. Relationship between eosinophils and asthma [J]. Chinese Journal of Ophthalmology and Otolaryngology, 2022, 22(1):102-105. DOI:10.14166/j.issn.1671-2420.2022.01.026.
[2] DOI: 10.1002/lary.32259
[3] Lai Kefang, Zhan Wenzhi, Jiang Ziyu, et al. A multicenter prospective observational study on the clinical characteristics, airway inflammation features and prognosis of cough variant asthma in China [J]. Chinese Journal of Tuberculosis and Respiratory Diseases, 2025, 48(11): 1009-1019. DOI: 10.3760/cma.j.cn112147-20250402-00180.
[4] Lin J, et al. J Asthma. 2014;51(1):34-43.
[5] Wang Yuqing, et al. Chinese Journal of Practical Pediatrics, 2022, 37(9):7.
[6] Chinese Society of Respiratory Diseases. Chinese Journal of Tuberculosis and Respiratory Diseases, 2025, 48(3): 208-248.