Why is sinusitis a hidden key factor in the difficulty of preventing and treating asthma?
Sinusitis (especially chronic sinusitis with nasal polyps, CRSwNP) is not only a common disease in otolaryngology, but also a "silent killer" affecting the health of the entire airway. Studies show that 43% of patients with severe asthma also have CRSwNP, and the presence of nasal polyps is significantly correlated with the severity of asthma. More alarmingly, sinusitis can be a trigger for new-onset asthma and worsen existing asthma.
1. Pathological commonalities between sinusitis and asthma
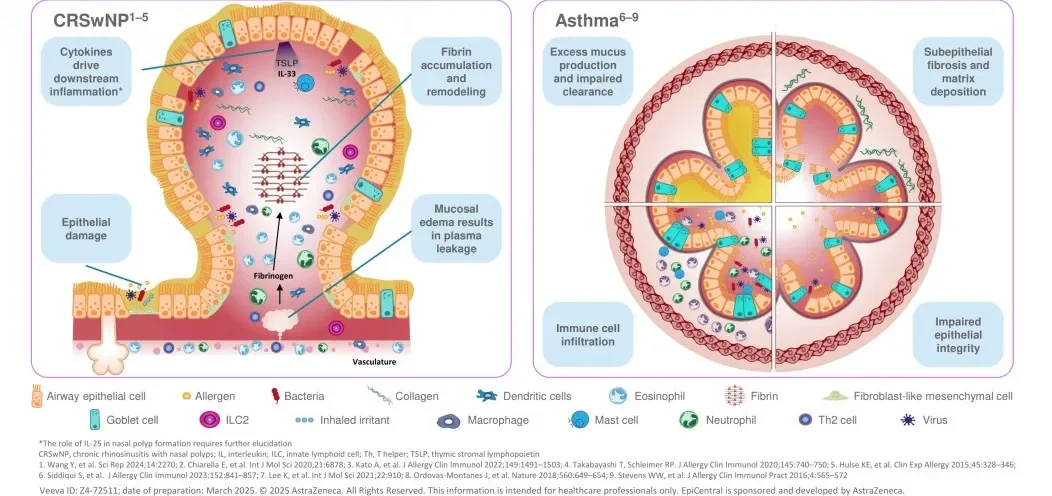
Sinusitis and asthma share certain pathological mechanisms, primarily involving epithelial barrier dysfunction and the joint participation of Th2-type inflammatory responses. Studies have shown that the sinus and bronchial mucosa are embryologically homologous and both are susceptible to Th2-type inflammation (such as IL-4, IL-5, and IL-13). The nasal mucosal epithelial barrier is damaged in patients with chronic sinusitis, similar to the thickening of the airway basement membrane in asthma patients, forming an "upper and lower airway inflammatory cycle." Bronchial biopsy studies further confirm that in patients with severe asthma complicated by sinusitis, both the upper and lower airways exhibit significant eosinophilic infiltration and high IL-5 expression.
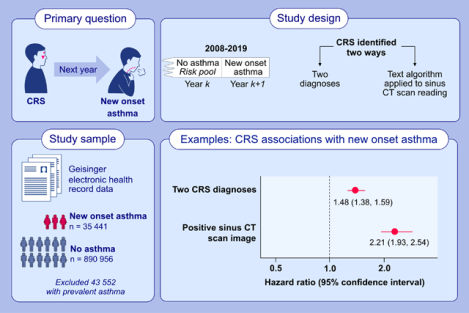
Epidemiological studies provide more direct evidence for this association: a large cohort study involving 35,000 people showed that patients with chronic sinusitis had a significantly increased risk of developing new-onset asthma the following year (OR=2.21, 95%CI: 1.93-2.54). The potential mechanisms may involve two aspects: first, the inflammatory secretions caused by postnasal drip directly irritate the lower respiratory tract; second, airway hyperresponsiveness is enhanced through the nasobronchial reflex pathway. These findings not only deepen our understanding of the "one airway, one disease" theory but also provide important clues for the early identification of high-risk groups for asthma.
2. Clinical implications of sinusitis exacerbating asthma
More notably, asthma patients with concurrent chronic sinusitis often face more severe clinical challenges: significantly reduced lung function (FEV1), persistently elevated type 2 inflammatory markers (FeNO, BEC), increased steroid dependence, and more frequent acute exacerbations. This "double whammy" is not only reflected in physiological indicators—the superposition of symptoms such as nasal congestion, olfactory dysfunction, wheezing, and dyspnea—but also leads to a significant deterioration in patients' quality of life scores (such as SNOT-22 and ACQ-7).
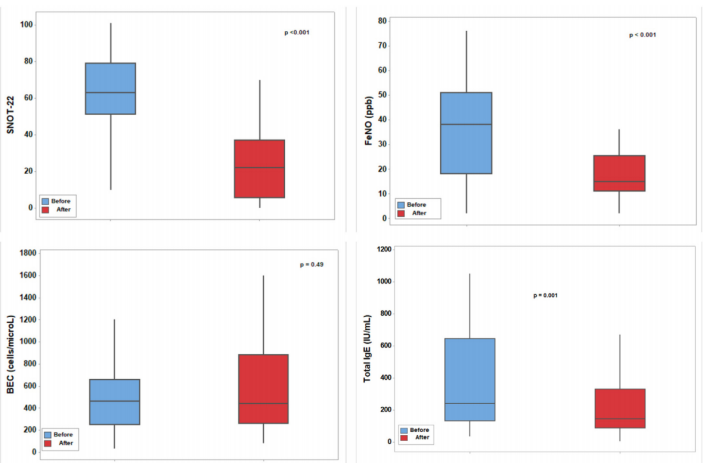
For this group, controlling sinusitis is key to improving asthma prognosis. Both nasal corticosteroids, biologics, and surgical interventions such as nasal polyp removal can effectively relieve symptoms. Studies have found that sinus surgery in CRSwNP patients can reduce the risk of acute asthma exacerbations by 40%. In the field of targeted therapy, a two-year prospective cohort study confirmed that dupilumab not only significantly improved symptoms, inflammatory markers, and imaging findings in CRSwNP patients, but also simultaneously optimized asthma outcomes (increased FEV1 and decreased FeNO). Notably, although CRSwNP patients with asthma had larger nasal polyps, their symptom improvement was comparable to that of patients with CRSwNP alone, with 7.3% of asthma patients ultimately achieving clinical remission. These findings provide important evidence for precision treatment of diseases affecting the same airway.
3. Precision diagnosis and treatment with integrated upper and lower airway management
Asthma combined with sinusitis is not merely a simple superposition of diseases, but rather a manifestation of the complex interaction of inflammatory mechanisms in the upper and lower airways. The integration of anatomical and immune aspects means that when the upper airway (such as the sinuses) is stimulated by allergens or pathogens, alarm factors released by epithelial cells (such as TSLP, IL-33, and IL-25) can simultaneously drive inflammation in the lower airways, creating an "inflammatory resonance." Furthermore, the coexistence of type 2 and non-type 2 inflammation further increases disease heterogeneity, making it difficult for traditional diagnostic and treatment methods to comprehensively assess the inflammatory status.
Against this backdrop, combined upper and lower airway expiratory NO testing (FnNO+FeNO) has become a key tool to overcome the limitations of blood tests or imaging (such as systemic interference from BEC and IgE) due to its high airway specificity . For patients with sinusitis, FnNO/FeNO monitoring can identify latent airway inflammation early and provide early warning of the risk of new-onset asthma; for patients with asthma and sinusitis, dynamic monitoring can optimize treatment plans, improve treatment adherence, and reduce the risk of acute exacerbations, providing a new direction for the precise management of diseases in the same airway.
References:
1.Fokkens W, Reitsma S. Unified Airway Disease: A Contemporary Review and Introduction. Otolaryngol Clin North Am. 2023 Feb;56(1):1-10.
2.Schwartz BS, Pollak JS, Bandeen-Roche K, et al. Sinus inflammation and chronic rhinosinusitis are associated with a diagnosis of new onset asthma in the following year. Allergy. 2023;78(10):2659-2668.
3.Al-Ahmad M, Ali A, Talat W, Dawood HA, Imam O. Long-term effects of dupilumab on chronic rhinosinusitis with nasal polyps: A step towards clinical remission. World Allergy Organ J. 2025;18(2):101024. Published 2025 Jan 16.